Thickened Nuchal Fold in Fetus
This blog explains what a thickened nuchal fold is, why it may occur, what tests your doctor may recommend, and what it can mean for your baby.
(Note: A thickened nuchal fold is a second-trimester ultrasound marker, different from the first-trimester “nuchal translucency” or NT.)
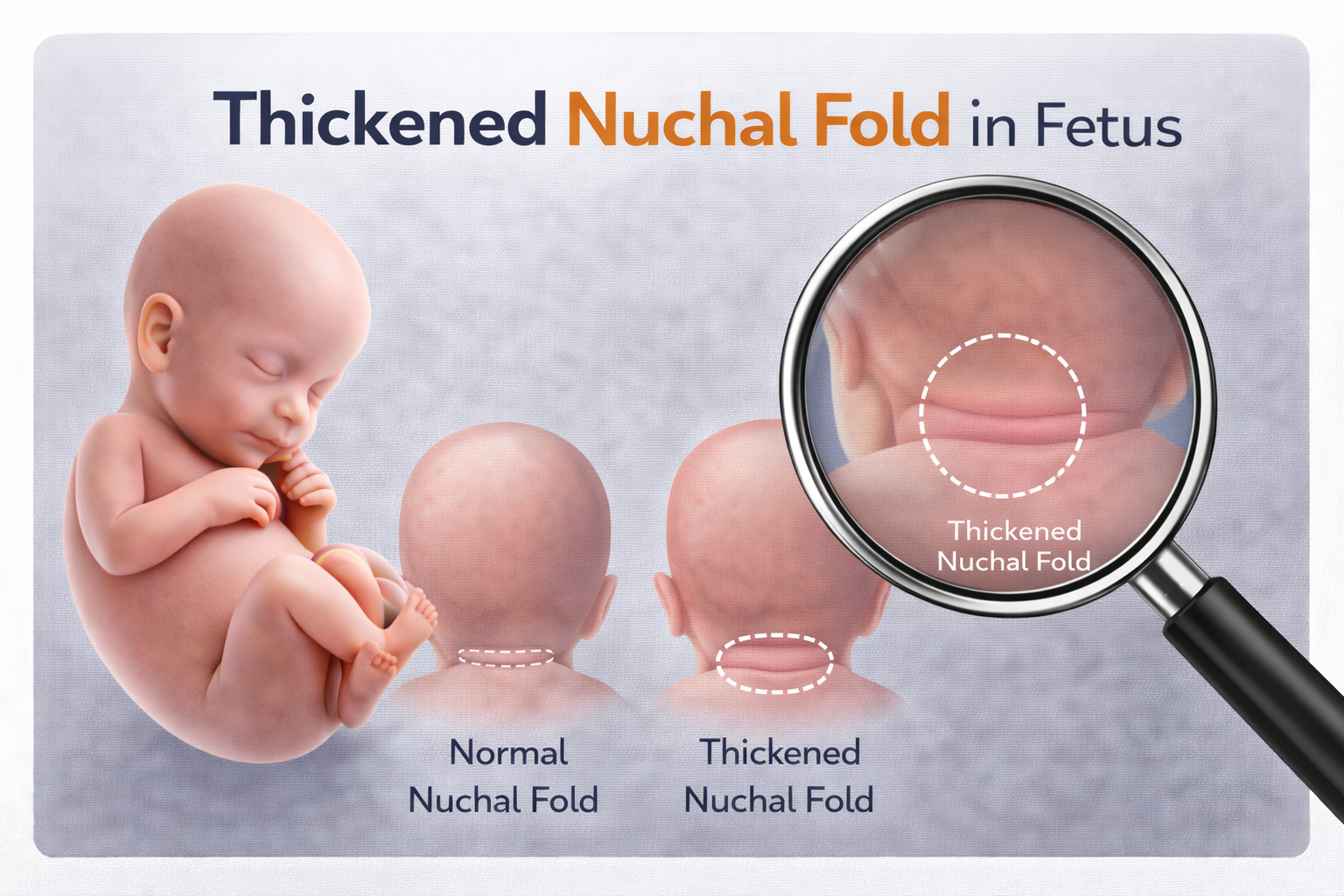
What Is the Nuchal Fold?
The nuchal fold is the layer of skin and soft tissue at the back of your baby’s neck. It is measured by ultrasound between 16-24 weeks of pregnancy. All babies have some thickness here – this is completely normal.
A thickened or increased nuchal fold means the measurement is more than 6 mm.
This does not mean your baby definitely has a problem. It simply increases the chance of certain conditions and suggests that further assessment may be helpful.
Why Can the Nuchal Fold Be Thickened?
A thickened nuchal fold can occur because of changes in how tissues and fluid develop or drain in the baby’s neck area. Possible reasons include:
• Altered extracellular matrix (ECM) – changes in connective tissues
• Disturbed lymphatic development – affecting how fluid drains
• Cardiac dysfunction – reduced heart function can cause fluid build-up
These mechanisms are often linked with, or occur alongside:
• Chromosomal conditions (e.g., Down syndrome – an extra chromosome 21)
• Single-gene disorders (such as Noonan syndrome)
• Heart defects
• Other structural differences seen on ultrasound
• Certain fetal infections
A thickened nuchal fold is seen in about 1 in 20 pregnancies, but only 1 in 10 of these babies will actually have an underlying problem.
Because of this, your doctor may recommend further tests to better understand your baby’s health.
Why Is Genetic Testing Important?
Genes and chromosomes contain the instructions for your baby’s growth and development.
Most people have 46 chromosomes (23 pairs).
An extra or missing chromosome – or certain single-gene changes – can lead to conditions such as:
• Down syndrome (Trisomy 21)
• Edwards syndrome (Trisomy 18)
• Patau syndrome (Trisomy 13)
• Some single-gene conditions
These conditions can affect development in different ways.
Should I Have Further Tests?
Many parents choose further testing to get clearer information.
Your doctor will discuss the options with you.
Genetic Tests
These tests examine your baby’s chromosomes and genes:
• NIPT (Non-Invasive Prenatal Testing)
– A blood test from the mother
– Screens for common chromosome problems
– Useful for screening, but not diagnostic
• Amniocentesis
– A small sample of the fluid around the baby is taken
– This is the confirmatory diagnostic test
These tests can detect:
Extra or missing chromosomes, Microdeletions,
Single-gene conditions (e.g., Noonan syndrome)
Types of genetic testing include
Karyotyping, Chromosomal microarray, Single-gene or targeted testing, including whole exome sequencing
Detailed Fetal Scan and Fetal Echocardiography
These specialized ultrasounds assess:
• All of baby’s organs and the structure and function of the heart
Testing for Fetal Infections
Your doctor may recommend tests to rule out certain infections that can affect the baby.
Follow-up During Pregnancy
Your doctor may suggest repeat scans later in pregnancy to:
• Monitor your baby’s growth
• Look for any new findings
• Check the amniotic fluid levels
A range of genetic tests may be used, including FISH, Q-f PCR, Karyotyping, Microarray analysis, and whole-exome sequencing. The final decision about which tests are most suitable will be made after evaluating multiple factors relevant to your case.
Things to Watch For
If all tests are normal, your pregnancy is generally considered low-risk.
However,
• The nuchal fold was very large – in some cases this can lead to hydrops fetalis, a condition involving fluid build-up in the baby and increased risk of complications.
• Mother abdomen begins to grow very quickly, which may indicate too much amniotic fluid (polyhydramnios). Polyhydramnios can occasionally be associated with conditions such as Noonan syndrome.
What Does a Thickened Nuchal Fold Mean After Birth?
• If all prenatal tests were normal, the chances of baby having normal growth and development are very reassuring.
• If a specific condition was identified, the outcome depends on that diagnosis.
• Occasionally, mild conditions not visible during pregnancy may become noticeable only after birth.
Will It Happen in Future Pregnancies?
Most of the time, a thickened nuchal fold does not recur in future pregnancies.
Your risk may be slightly higher if:
• A previous baby had a chromosomal or single gene condition
• A previous baby had a heart defect
- Choroid Plexus Cyst
- Who is at Risk?
- Down Syndrome
- Thickened Nuchal Fold in Fetus
- Absent or Small Nasal Bone
- Echogenic intracardiac focus (EIF) in the fetal heart
- Cerebellar hypoplasia (CH) in Fetus
- Agenesis of Septum Pellucidum in Fetal Brain
- Ventriculomegaly in the Fetal Brain
- Mega Cisterna Magna – MCM

Committed to precise diagnostics, empathetic guidance, and advanced fetal care — supporting mothers and babies at every step of their journey.
Quick Links
Contact Information