Understanding Mega Cisterna Magna (MCM) Genetic soft marker
This blog is designed to help you understand what Mega Cisterna Magna (MCM) is, what tests may be suggested during pregnancy, and what it may mean for your baby after birth.
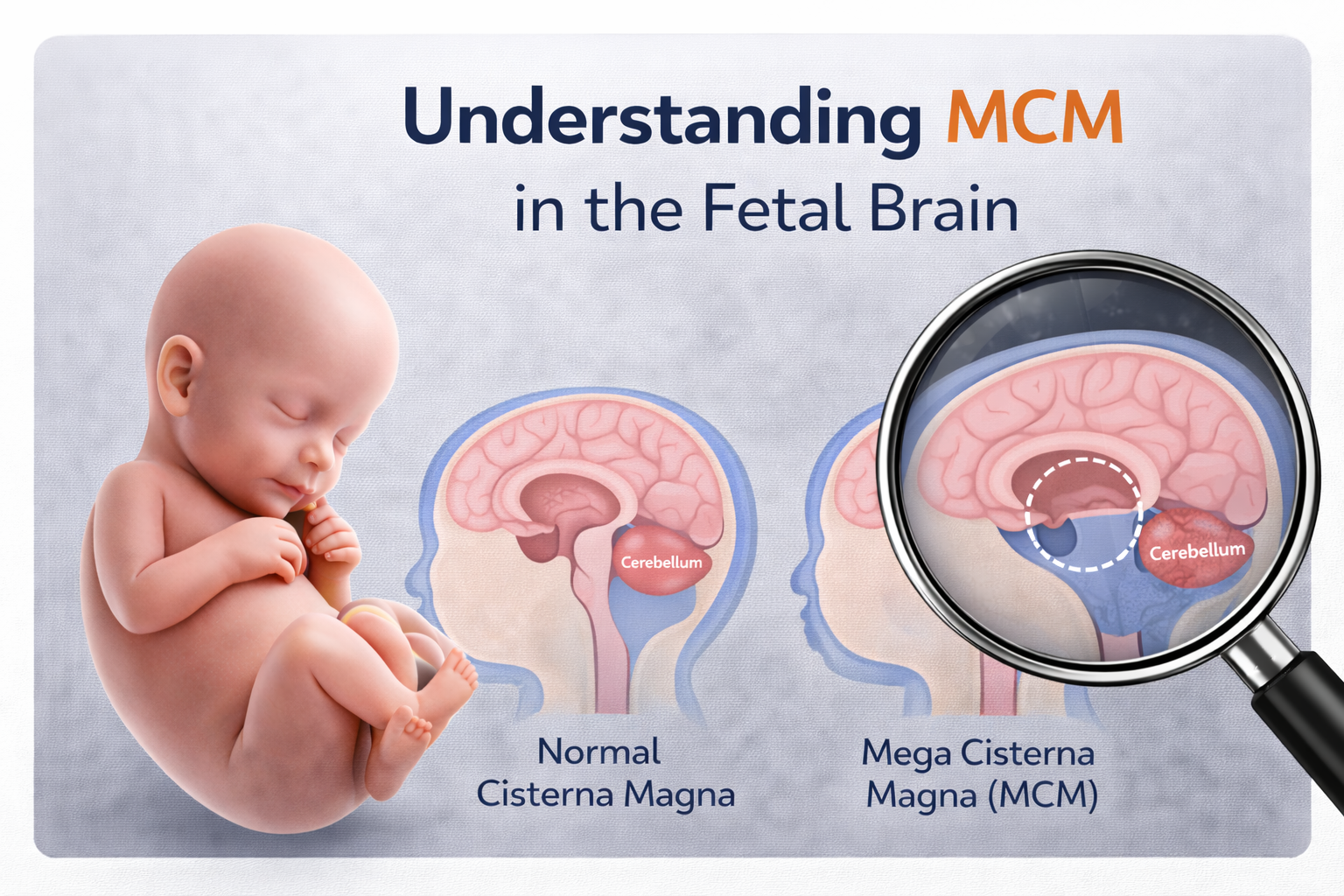
What is Mega Cisterna Magna (MCM)?
The cisterna magna is a normal, fluid-filled space located at the back (posterior part) of the brain. In MCM, this space is larger than usual without any other major structural differences in the brain.
How does MCM happen?
During early fetal development, the spaces that carry cerebrospinal fluid (CSF) .If this process varies slightly, CSF may collect more in the cisterna magna, making it bigger than normal.
Possible Reasons for MCM
MCM can happen due to several reasons, including:
- Isolated normal variant – Many babies with isolated MCM are healthy.
- Chromosomal abnormalities, such as Trisomy 13 or Trisomy 18.
- Single-gene disorders (much less common).
- As part of a group of developmental differences in the brain.
- Viral Infections, such as cytomegalovirus (CMV), in some cases.
Chromosomes carry our genetic information. Most people have 46 chromosomes arranged in 23 pairs. About 3,000 genes are stored on these chromosomes. Rarely, a baby may have an extra chromosome or a change in a gene, and this can be associated with MCM.
How is genetic testing relevant to an MCM
Research shows that when MCM is truly isolated, the chance of a genetic abnormality is low. Genetic testing is more likely to be recommended when:
- MCM is not isolated
- other brain or organ differences are seen, or
- Concerns arise during the overall evaluation.
The specific type of testing depends on multiple factors and the findings in your baby.
What additional tests may be required?
Your healthcare team may suggest extra tests to understand the condition more clearly, such as:
- Detailed ultrasound to check the baby’s full anatomy, including the heart
- Neurosonography, a specialised ultrasound that gives a closer look at the brain
- Fetal MRI to look for subtle brain changes and confirm that nearby structures are normal
- Genetic testing, which may be recommended if other abnormalities are found
Types of genetic testing procedures which are generally offered are:
- Non-invasive prenatal testing (NIPT)
- Amniocentesis for fetal genetic testing
Genetic diagnostic tests that may be used include:
- FISH
- QF-PCR
- Karyotyping
- Microarray analysis
- Whole-exome sequencing
Your healthcare consultants will select the most appropriate tests after considering all findings and relevant factors.
What should be monitored during pregnancy?
MCM may:
- Change in size over time
- appear temporarily, or
- become more noticeable as the fetus grows.
Follow-up ultrasounds are recommended to watch the cisterna magna and ensure that other brain structures continue to appear normal.
What does MCM mean for my baby after birth?
After birth, a brain ultrasound is usually performed to confirm the diagnosis and check brain anatomy. Most babies with isolated MCM have normal development.
Will this happen again in future pregnancies?
- If no genetic cause is found, the chance of MCM occurring again is low.
- If a genetic condition is identified, the chance of recurrence depends on the specific diagnosis.
A consultation with a genetic specialist or fetal medicine specialist can offer guidance and counseling for future pregnancies and help ease any worries about the chance of recurrence.
Disclaimer
This blog provides general information only. It is not medical advice and should not replace the personalised guidance, diagnosis, or treatment offered by your healthcare professionals.
- Choroid Plexus Cyst
- Who is at Risk?
- Down Syndrome
- Thickened Nuchal Fold in Fetus
- Absent or Small Nasal Bone
- Echogenic intracardiac focus (EIF) in the fetal heart
- Cerebellar hypoplasia (CH) in Fetus
- Agenesis of Septum Pellucidum in Fetal Brain
- Ventriculomegaly in the Fetal Brain
- Mega Cisterna Magna – MCM

Committed to precise diagnostics, empathetic guidance, and advanced fetal care — supporting mothers and babies at every step of their journey.
Quick Links
Contact Information